
Cervical spondylosis (CS) is one of the most common diseases of the musculoskeletal system. Every year doctors diagnose this disease more and more often, and its course becomes more and more severe. According to statistics, in women, degeneration and dystrophy in the upper spine occurs more often, especially in postmenopausal patients. The main symptoms of cervical spondylosis in women are pain, limited movement, and cerebrovascular insufficiency, which is dangerous not only for health but also for life. To protect yourself from the dangerous consequences of pathology, you need to start treatment at an early stage. It is important to carry out complex therapy and lifestyle changes to stop the destruction of spinal segments and prevent serious complications.
Development of the disease
The cervical spine is most vulnerable to various injuries and degeneration. This is because this segment is the most mobile and the muscles here are weak. The small cervical vertebrae are subjected to heavy loads every day, leading to the gradual destruction of the intervertebral disc. The vertebrae put pressure on each other, causing the cartilage between them to lose a lot of fluid and begin to degenerate and deform.
In addition, cervical spine cartilage degeneration also develops due to insufficient nutrition of cartilage tissue. And the spinal canal in this area is narrow, so it is often compressed, causing neurological symptoms.
The disease in women in the early stages is manifested by heaviness in the back of the head, tingling in the hands, etc. Patients often confuse the first signs of the disease with fatigue.
There are many blood vessels and nerve roots in the neck area, and when they are compressed, neurological disorders can occur. This is especially dangerous if a deformed disc or vertebra presses on the vertebral artery, which supplies blood to important parts of the brain. When it is compressed, coordination of movements is impaired, a woman may lose balance, vision and hearing deteriorate, and the risk of stroke increases.
Authority to solve.According to statistics, cervical spondylosis is most common in patients aged 25-40 years. This is due to a large decrease in physical activity and sedentary work. Women are more often diagnosed with this disease than men because they have more fragile vertebrae and thin bone tissue.
Doctors distinguish 4 stages of spinal degeneration:
- State 1– the disc loses some of its moisture, its height decreases, and cracks may appear on the annulus (outer shell). This is the stage of cervical cartilage disease, which is difficult to determine because there are no symptoms. The neck quickly gets tired, there is a feeling of discomfort and heaviness in the damaged area, sometimes there is a slight pain that quickly passes.
- Phase 2– cracks on the disc surface increase, the nucleus pulposus (gel-like substance of the disc) shifts and can protrude through damaged areas. This is how cartilage protrusions appear, which can compress the spinal cord and its roots. Severe pain, weakness, limited movement sometimes appear and there may be numbness of the face, neck, shoulders and arms.
- Stage 3– The protruding part penetrates the outer shell of the disc, forming a herniation. The pain becomes more pronounced and neurological disorders appear.
- Stage 4– the intervertebral disc is almost completely destroyed, the vertebrae rub against each other and bone growths (osteoporosis) appear on their edges, aimed at stabilizing the damaged segment. Nerve endings, spinal cord and blood vessels are violated. Adjacent joints begin to hurt. Clinical signs are pronounced.
The easiest way to prevent degenerative-dystrophic changes in the first two stages of spondylolisthesis. In stage 3, comprehensive treatment will help prevent further destruction of the spinal segment. In the final stages, surgery cannot be avoided.
reason
Spinal degeneration is a complex and prolonged process, often with many causes. In most cases, pathology occurs due to a sedentary lifestyle, poor nutrition and metabolic disorders. Usually the disease occurs due to injury or due to the natural aging of the body and weakening of defenses.
Doctors identify the main causes of spinal degeneration in women:
- Violation of metabolic processes.
- Passive lifestyle.
- Genetic predisposition.
- Chronic muscle tension around the cervical segment.
- Distortion of posture.
- The body lacks fluids and nutrients.
- Staying for a long time in an uncomfortable position (neck stretched forward and back bent).
- Excessive weight.
- Frequently wear high heels.
- SHOP injured.
- Lift heavy objects.
- Autoimmune disease.
- Frequent stress and chronic fatigue.
- Hypothermia.
- Infectious Diseases.
- The neck is too long or short, etc. v.
All these factors cause malnutrition of the intervertebral disc and lead to disc degeneration.
Cervical spondylosis in women can be caused by vertebral artery diseases related to genetic factors, uterine disorders and trauma during childbirth. The disease can occur due to rheumatism, endocrine disorders, excessive load on the cervical segment during pregnancy and local overload.
Important.The main cause of cervical spondylosis in women is menopause, as well as changes related to this period. At this stage, progesterone levels in the body decrease, which is important for bone tissue. The possibility of degenerative changes is associated with age-related weakening of the neck muscles and weakening of vertebral support in this area.
Symptom
Osteonecrosis is characterized by a wave-like course, when the acute phase is replaced by remission. Aggravation of the condition can be caused by infection, trauma, hypothermia, and prolonged muscle tension in the neck.

The first signs of cervical spondylosis in women are headaches, discomfort and heaviness in the neck. It is important to promptly distinguish cartilage pain from migraine or autonomic dysfunction.
Clinical manifestations of cervical spondylosis in women are due to neurological syndromes:
- Cervical pain occurs when nerve endings are irritated by damaged pieces of cartilage. Then a specific spasm in the neck appears, the pain becomes more pronounced when moving the head and after sleep.
- Squamous syndrome results from damage to the blood vessels and nerves of the brachial plexus and subclavian artery. This symptom complex is accompanied by pain from the inner surface of the shoulder to the hand on the injured side. The limbs become pale, cool, swollen and numb. Neck pain spreads to the back of the head when the patient turns his head.
- Periarticular shoulder syndrome - dystrophic changes affecting the tendons that surround the shoulder. The pain spreads from the neck to the shoulder and shoulder blades. The neck has a forced posture - tilted towards the affected side and the shoulders slightly lowered.
- Vertebral artery syndrome - blood vessels are compressed by damaged disc fragments or bone spurs (depending on the stage of the disease). Patients feel dizzy, headache, nausea and sometimes vomit. The pain is localized in the back of the head, top of the head and temples.
- Heart – nerve bundles of the spinal cord are damaged. Heart attacks and arrhythmias occur. If C3 is damaged, a migraine will occur, the tongue will swell, and the patient will not be able to chew food normally. If C4 is injured, discomfort appears in the shoulder girdle, collarbone and heart. When C5 is affected, the pain response spreads from the neck to the shoulder girdle, the inside of the shoulder. Stimulation of C6 causes pain from the neck and shoulder blades to the shoulder girdle and radiates across the arm to the thumb. If C7 is damaged, the pain syndrome spreads behind the shoulder girdle, affecting the entire hand, including the index and middle fingers. When C8 is compressed, pain radiates from the affected area to the elbow and little finger.
In addition, the woman's emotional sphere may be disturbed, weakness may occur, she becomes nervous and emotional. Insomnia often occurs, memory and attention are weakened due to frequent headaches.
Symptoms of a stroke occur when a woman suddenly throws her head back, tilts her head, or performs tasks that put stress on the arms and cervical spine, such as digging or painting. ceiling or carrying heavy objects.
Poor cerebral circulation is manifested by dizziness, unsteady gait, spots before the eyes, tinnitus, weakness, and nausea. In some patients, the voice becomes hoarse, sometimes disappears, and a sore throat appears.
Cartilage degeneration during menopause is accompanied by migraines and increased sweating in the area between the neck and shoulders. When the vertebral artery is compressed, the activity of the cardiovascular system is disrupted.
If the disease persists, circulatory failure occurs in important centers that perform neuroendocrine functions. Due to increased permeability of the vessel walls, atherosclerosis in the arteries of the brain and heart develops.
Establish diagnostics
If you notice symptoms of osteonecrosis, see a therapist. After a visual examination, the specialist will refer you to an orthopedist, spine specialist or neurologist.
The following methods are used to diagnose cervical spondylosis:
- X-rays allow us to detect that the patient's vertebrae are displaced, there are bone spurs at the edges, the distance between the vertebrae has decreased, etc. v. To do this, research is carried out on different planes. To detail characteristic changes, your doctor will take targeted pictures.
- CT scan of the cervical spine provides detailed information about pathological changes in the vertebrae. This method allows you to obtain three-dimensional images for more detailed study, it is used in serious diagnostic cases.
- MRI is used to accurately assess the condition of soft tissues (nerves, blood vessels, ligaments, muscles) in the affected area.
- Electromyography allows you to test the conductivity of nerve fibers.
Doctors may also prescribe an ultrasound (Doppler ultrasound of the main arteries of the brain) to determine the state of blood flow in this area.
Conservative treatment
In the early stages, treatment of osteoarthritis of the spine in women can be done at home. However, the doctor must provide a treatment regimen. It is important to understand that this is a long process and full recovery is unlikely (especially for older women).
Complex treatment includes:
- Are taking medication.
- Use orthopedic devices.
- Physical therapy.
- Physical therapy procedures.
- Massage, manual action.
- Alternative treatments.
Conservative methods will help reduce pain, inflammation, normalize muscle tone, improve metabolism, nutrition of damaged spinal segments, etc. v. If treated promptly, pathological changes can be prevented.

Treatment of cervical spondylosis in women is carried out using drugs that improve the metabolism of the cartilage pads between the vertebrae, reducing inflammation and pain. The following drugs are used for this purpose:
- NSAIDs. They will help reduce mild or moderate inflammation and pain.
- Analgesic. Pain relief.
- The drug improves cerebral circulation.
- Muscle relaxants help reduce muscle spasms.
- Chondroprotectors. They help prevent disc destruction, improve metabolism and speed up recovery.
- Medicines based on magnesium.
- Nootropics. They stimulate brain activity by normalizing blood circulation and have a mild sedative effect.
Authority to solve.For severe pain that is not relieved by oral medications, such as anesthetic blockade therapy or NSAIDs.
Treatment can be supplemented with anti-inflammatory and pain relievers in the form of gels, creams and ointments. They will be effective in the remission phase or in combination with oral medications.
The decision to choose a drug combination is made by the doctor. The specialist will draw up a medication regimen and determine their dosage. It is important to follow his recommendations, since many of the drugs described above can lead to dangerous complications.
During the acute stage of osteonecrosis of the spine, a woman should refuse heavy physical activity. To reduce the neck, you need to wear a special corset (Schants neck), which will fix the vertebrae in the correct position. This device is recommended for use during periods of sedentary activity or heavy work.
Physiotherapeutic procedures will help relieve pain and improve blood circulation in the damaged area:
- Diadynamic therapy.
- Magnetic therapy.
- Electrophoresis with anesthetics, glucocorticosteroids, proteolytic agents.
- Electric pain relief.
- Ultraviolet radiation, etc. v.
The therapeutic effect appears approximately after the third session, then headaches, hearing and visual disorders, dizziness weaken or disappear, sleep returns to normal and the general condition improves.
Using underwater traction of the cervical segment, you can widen the space between the vertebrae, free the nerves or blood vessels from compression, and restore the normal position of the vertebrae.
Massage will normalize muscle tone and reduce the flow of lymph fluid, which causes swelling. After several sessions, blood circulation in the damaged area improves.
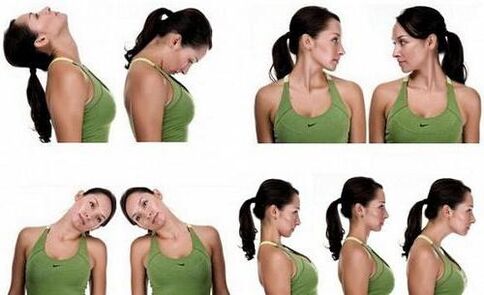
Physical therapy is one of the most effective treatments for spinal degeneration. Exercise therapy allows you to strengthen weak neck muscles, which will then take on part of the load from the spine and help prevent or slow down degenerative changes. During training, blood circulation improves, metabolism and disc nutrition are accelerated, which has a positive effect on their condition.
Women should exercise every day. They include simple but effective exercises. The complex includes movements of rotation, tilting the head in different directions, as well as movements of the neck, in which the arms are used. These elements can be performed at home, but only after approval from your doctor. Physiotherapy is carried out only at the stage of remission.
Complex treatment can be supplemented with acupressure (acupuncture), hirudotherapy (leech treatment), swimming, etc. v.
Surgery
This surgery is indicated in the final stages of osteochondrosis of the spinal cord, which is accompanied by severe destruction of bone and cartilage structures. In addition, surgical intervention cannot be avoided if conservative methods are ineffective or the spinal canal is significantly narrowed.
In the above cases, anterior cervical resection is performed. During the procedure, the doctor will immobilize the damaged spinal segment and remove the herniated part that is compressing the spinal nerves. The vertebrae between the removed discs are then fused. If necessary, the space between the vertebrae will be filled with a synthetic insert (cage).
After 3-5 days the patient is discharged home. Recovery time is about 12 weeks. To speed up recovery, you need to take medication, wear a corset, lead a healthy lifestyle, undergo physical therapy and finally perform exercise therapy.
Lifestyle recommendations
To quickly get rid of unpleasant symptoms of osteoarthritis and prevent degenerative-dystrophic changes in the neck segment, you need to adjust your lifestyle. To do this, the patient must follow the following recommendations:
- Go for a walk every day, avoid running, jumping and other explosive activities.
- Do not carry heavy objects.
- You cannot sit for a long time, in severe cases, wear a corset and periodically lie horizontally.
- Do special physical exercises for back muscles at home.
- Sleep on an orthopedic mattress and a special pillow.
- Going on a diet, supplement your diet with foods rich in magnesium, calcium (nuts, dairy products, seafood, legumes), as well as vegetable fiber, chondroitin (jelly meat, jelly). Avoid fatty, fried, overly salty foods and alcohol. The doctor will advise in more detail about nutritional rules. But in any case it must be true.
Hypothermia is not allowed, warming up will be beneficial in the absence of an inflammatory process.
symptoms
In case cervical spondylosis is not treated promptly, a woman may experience the following pathological consequences:
- The possibility of protrusion, after a while, will turn into a hernia. The bulge compresses the spinal cord as well as its nerves, causing neurological disorders.
- Osteoporosis occurs when the intervertebral disc is severely damaged and causes irritation to the spinal nerves and blood vessels.
- In severe cases, there can be severe weakness of the neck muscles or incomplete paralysis, in which the head involuntarily tilts to one side or forward.
- Compression of the vertebral arteries, circulation is impaired in the affected area. This condition can cause neuralgia (pain along the nerves), hearing and vision problems.
- Paralysis (incomplete or complete) of the hand.
- Cerebral stroke, etc. v.
If a woman addresses this problem in the early stages of spinal osteonecrosis, she will be able to prevent the conditions described above.
Precautions
Ideally, prevention of spinal osteonecrosis should be done during the period of intrauterine development. The future mother must exclude factors that negatively affect the development of the fetus: infection, lack of oxygen, intoxication. If there is trauma at birth, the newborn must be treated.
To reduce the likelihood of developing spondylolisthesis, women should follow these recommendations:
- Load your spine evenly, such as carrying the load with both hands or alternating on the right then the left.
- Don't lift too heavy weights on your own.
- Try to avoid neck injuries and hypothermia.
- When working on the garden plot, take a break every 1. 5 hours and lie down for 20 minutes.
- Choosing shoes with elastic soles will reduce impact when running or jumping.
- When sitting for long periods of time, use a high-backed chair with a headrest or wear a corset.
It is also important to eat properly, control weight, avoid stress, take vitamin supplements for medical reasons and promptly treat diseases that can cause osteoarthritis. During the period of remission, it is recommended to go to sanatoriums to undergo a course of treatment.
The most important thing
As you can see, cervical spondylosis occurs more often in women than in men, because women have more fragile vertebrae and thin bone tissue. Patients in the postmenopausal period are especially susceptible to the disease. The disease is manifested by pain, neurological disorders as well as dangerous symptoms of stroke. Treatment should be started in the early stages to avoid dangerous complications of osteoarthritis. To do this, a woman must take medication, adjust her lifestyle, participate in physical therapy, massage, physical therapy, etc. v. Surgical treatment is indicated only in severe cases. To prevent pathology, you need to maintain moderate physical activity, promptly treat injuries and diseases that can cause osteoarthritis, etc. v.



























